- +91 91000 65552
- +91 9324982134
- contact@respliceinstitute.com
- Mon-sat 10:00 -18:00
Your gut is like a tube, which is long and has many twists. It is covered in a soft, absorbent carpet-like layer that helps your body soak up nutrients from food. Now imagine that parts of this carpet are swollen, red, and painful, as if they’ve been scratched or burned from the inside. That’s what Inflammatory Bowel Disease (IBD) is.
It’s a long-term illness where your body’s own immune system mistakenly attacks the intestines, causing inflammation. Unlike Irritable Bowel Syndrome (IBS), which doesn’t cause damage, IBD actually harms the digestive tract over time.
It’s not just a “stomach issue.” IBD is a full-body challenge that can affect your growth, energy, mood, and even how your joints or skin feel. It shows up differently in everyone, and flares may come and go, but the impact can be deeply personal and daily.

There are two main types of IBD. They’re like cousins—similar, but with key differences.
This can affect any part of the digestive tract, from the mouth to the anus. But it often targets the small intestine. It causes deep ulcers and thick inflammation that can go through several layers of the gut wall. Example: Imagine your food pipe is a garden hose, and Crohn’s creates patches of swelling, holes, and narrow parts along the hose. Water can’t flow well, and leaks may happen.
This affects only the large intestine (colon) and the rectum. The inflammation here stays on the surface layer but is often more widespread. Example: If the colon is a long hallway with soft wallpaper, Ulcerative Colitis peels the wallpaper off in long, continuous strips, causing pain, bleeding, and urgency.
Both fall under the larger spectrum of inflammatory bowel diseases, which are immune-mediated and need long-term care.
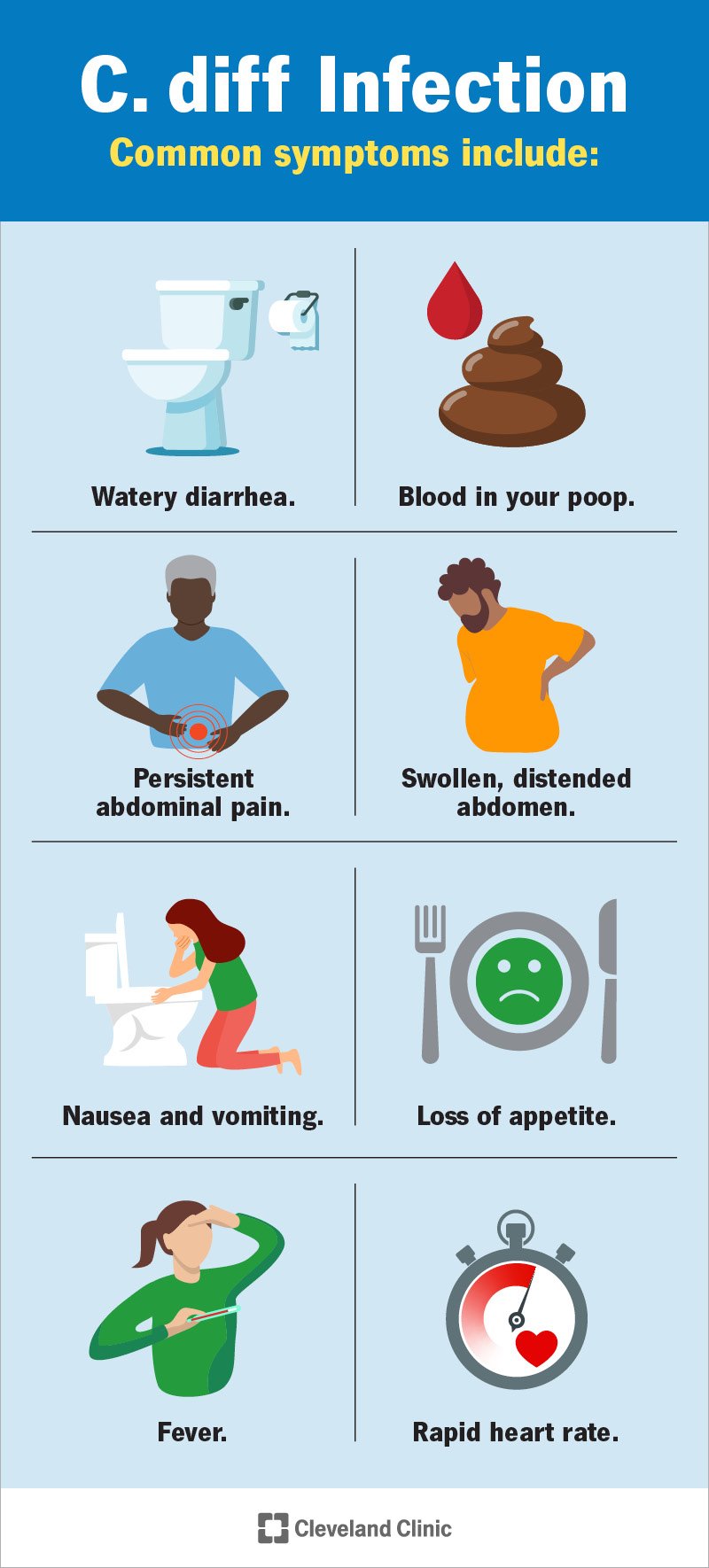
Depending on the severity and type, some symptoms vary, but some signs are classic:
Some also experience:
Sometimes, if untreated for a long time, it leads to anemia, dehydration, and hospitalization.
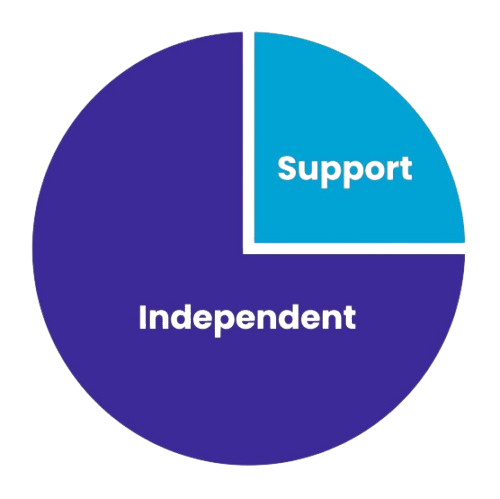
There’s no one “villain” behind IBD. Instead, it’s like a perfect storm of:
IBD tends to run in families. If a close relative has it, your risk increases.

In IBD, your immune system overreacts to things in your gut—like food, bacteria, or even your own tissues—causing damage.

When the balance of gut bacteria is off, inflammatory reactions may increase. This is known as gut dysbiosis in IBD and is a big area of research in gut microbiome treatment.

Pollution, poor diet, stress, antibiotics, or even infections might trigger IBD in those who are genetically prone.

But remember—it’s not your fault. Habits like laziness, or eating a lot of junk food, or something you did, don’t cause IBD. It’s a medical condition, and it needs medical support.
Doctors don’t rely on just one test. They look at your story, symptoms, and then dig deeper:

Check for inflammation, anemia, and nutrient deficiencies.

Check for signs of bleeding, infection, or gut inflammation (like calprotectin levels).
A camera is used to look inside the large intestine and take tiny samples (biopsies) to confirm IBD.

Used especially in Crohn’s to see inflammation in the small intestine or deep tissue damage.
Sometimes a gut microbiome test may be used to look for imbalances, especially when exploring gut-brain axis therapy, functional gut disorder diagnostics, or gut issues that may overlap.
Teenagers may be misdiagnosed as having IBS or “just anxiety” unless doctors dig deeper. That’s why early awareness and testing matter.
These are often supported by child development therapy centers, pediatric gastroenterology units, or autism gut health clinics when children or teens have overlapping symptoms.
Inflammatory Bowel Disease is a condition where the gut turns into a battlefield—but not all battles need to be fought with force. Some need balance, healing, and understanding. Whether it’s diet, medicine, microbiome therapy, or emotional support, the goal is always the same: to make peace within.
Resplice follows the International Stool Banking Consensus and goes beyond by adding gut microbiome and food intolerance testing. Donors are screened for -
Only children with excellent gut profiles are accepted.
Why use child donors under 12?
Fresh stool is -
Only the clear supernatant (fluid rich in good microbes) is used for colonic infusions
GMT isn’t one-and-done. It’s done in weekly sessions over several weeks, giving the new microbes time to settle, grow, and reshape the gut from the inside.
The goal? To help the gut communicate better with the brain, respond better to therapy, and reduce the pain, urgency, and exhaustion that IBD often brings.
At Resplice Research Institute, doctors are providing Gut Microbiota Transplantation (GMT) as a supportive treatment for people with Inflammatory Bowel Disease (IBD)—especially those with gut dysbiosis, poor response to medication, or who struggle with gut-brain axis imbalance.
The Big Idea: Our gut is like a massive ecosystem filled with tiny living organisms. In IBD, this ecosystem is usually out of balance, with too many inflammatory or harmful bacteria and not enough of the healing, calming kind.
GMT works by gently introducing healthy gut bacteria from a child donor into the intestines of the person with IBD. This re-seeds the gut with a better mix of microbes, which may:

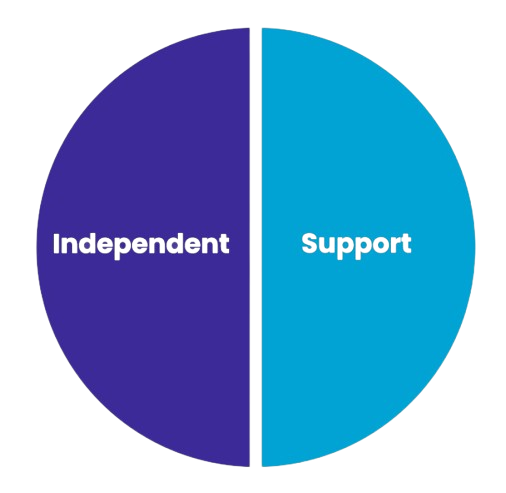
IBD is a chronic condition where the body’s immune system mistakenly attacks the digestive tract, causing inflammation. It’s not just a “gut issue”—it can affect your energy, growth, and even mental health.
While IBS causes discomfort, it doesn’t damage the gut. IBD, on the other hand, causes real inflammation and injury to the intestines that can be seen during tests like colonoscopy.
⦿ Crohn’s Disease: Can affect any part of the gut, often the small intestine; causes deep inflammation.
⦿ Ulcerative Colitis: Affects only the colon and rectum; inflammation stays on the surface but can spread widely.
Stomach cramps, diarrhea (often with blood or mucus), fatigue, weight loss, and urgency to poop—even when nothing comes out. Some people also have joint pain, rashes, or anxiety.
Yes, and it’s increasingly diagnosed in teens and young adults. It can affect growth, appetite, and mood. Early diagnosis is important, especially if it’s mistaken for IBS or anxiety.
A mix of genetics, immune system overreaction, gut bacteria imbalance (dysbiosis), and environmental triggers like diet, pollution, or stress. It’s not caused by lifestyle or food choices alone.
No. IBD is not contagious and has nothing to do with cleanliness. It’s an autoimmune condition—not a germ that spreads from one person to another.
Doctors use:
⦿ Blood and stool tests (for inflammation, anemia, infections)
⦿ Colonoscopy with biopsy
⦿ Imaging (MRI or CT) for deeper gut views
⦿ Sometimes gut microbiome testing
Gut dysbiosis means there’s an imbalance in good and bad bacteria. In IBD, this imbalance can worsen inflammation, symptoms, and even affect mood. Restoring balance is a key treatment goal.
GMT introduces healthy bacteria from screened child donors into the gut of someone with IBD. This may lower inflammation, reduce symptoms, and help the gut heal by restoring microbial balance.
Children’s microbiomes are less exposed to pollution, junk food, and antibiotics. Their gut bacteria are gentler and cleaner, making them ideal for rebalancing an inflamed gut.
No. GMT at Resplice is done in carefully spaced rounds. Each session helps the new bacteria settle in and multiply, slowly shifting the gut ecosystem toward healing.
Doctors may use anti-inflammatory drugs, immunosuppressants, biologic injections, dietary changes, and in some cases, surgery. These reduce symptoms and help manage flares.
IBD is a lifelong condition. While there’s no permanent cure, symptoms can be well-managed. With the right care—including gut therapy, nutrition, and emotional support—many people live full, vibrant lives.

Resplice Institute is India’s first integrated center offering autism therapy, gut microbiome treatment, and preventive health planning. We combine science and empathy to heal lives from the root.
© 2025 respliceinstitute.com || All Rights Reserved