- +91 91000 65552
- +91 9324982134
- contact@respliceinstitute.com
- Mon-sat 10:00 -18:00
Global Developmental Delay (GDD) is when a young child takes longer than expected to reach important milestones in more than one area of development.
Think of a child’s growth like a train journey. Each station is a milestone—like sitting, walking, talking, learning words, and playing with others. Most kids pass these stations around the same time. But a child with GDD is like a train running a bit late—it still moves, just slower, and might need extra help to catch up. It’s not the same as a child being lazy or just “slow.” The brain may be wired a little differently, and with the right support, many children with GDD can improve and thrive. Children showing signs like these are often referred for developmental delay therapy for children.
GDD is usually diagnosed in children under the age of 5 when delays are seen across two or more areas, such as:
Often, a team at a child development center works together to assess and plan the next steps.

GDD itself isn’t divided into “types” the way ADHD or autism are, but the areas in which a child is delayed give us clues to the type of support they need. Here’s how you can think about it:
a) Motor Delay: Struggles with body movements—like rolling, sitting, crawling, or walking. E.g., A child who hasn’t started walking at 2 years of age or can’t hold a spoon to feed themselves. They may benefit from occupational therapy or their local city, especially if therapy is focused on balance, grip, or motor planning.
b) Speech and Language Delay: Delays in understanding language or expressing themselves with words. E.g., A child who says only a few words by age 3 or doesn’t point to things they want. These are often addressed through speech therapy for children.
c) Cognitive Delay: Trouble with thinking, problem-solving, or remembering things. E.g., A child who can’t stack blocks, sort shapes, or understand basic instructions like “Give me the ball.”
d) Social or Emotional Delay: Difficulty with interacting, playing, or showing emotions. E.g., A child who doesn’t smile at familiar people, avoids eye contact, or doesn’t respond to their name.
e) Adaptive or Daily Living Delay: Struggles with everyday tasks like eating, dressing, brushing teeth, or using the toilet. E.g., A 5-year-old who still needs to be spoon-fed or shows no interest in toilet training.
Most children with GDD have a mix of these delays, not just one. That’s why it’s called “global”—it affects multiple areas. Early support through early intervention programs can help children build skills across all these domains.
Every child grows at their own pace, but if a child is much slower than expected in several areas, it could be GDD. Here are some common signs grouped by developmental areas:
There’s no single reason why a child develops GDD. It’s usually a mix of genetic, medical, and environmental factors. In many cases, doctors can’t find one clear cause. But early support can make a huge difference, even if the cause isn’t fully known.
Sometimes a child is born with a difference in their genes or chromosomes. E.g., conditions like Down syndrome or Fragile X syndrome can cause GDD. Doctors may recommend a genetic test for autism or GDD-related syndromes when appropriate.
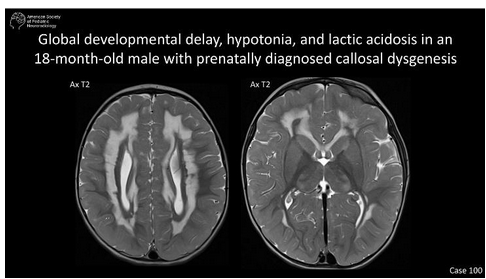
ssues in how the brain developed or got injured.
Problems during pregnancy like:
Some families may explore broader approaches, such as functional medicine, to investigate nutrient deficiencies, toxin exposure, or gut health that could contribute to developmental challenges.
Doctors use a step-by-step evaluation to check the child’s development. Here’s how it usually works:
A) Developmental Screening: Pediatricians use tools like the Denver II or ASQ (Ages & Stages Questionnaire) to compare the child’s development with typical milestones. E.g., “Can your child point to body parts when named?” “Can they stack two blocks?”—simple yes/no questions. This is often the first step in identifying developmental delay treatment needs.
B) Medical & Genetic Testing: If delays are significant, doctors might suggest:
C) Psychological & Educational Evaluation:
These evaluations may be done at a multidisciplinary rehabilitation center or early intervention clinic.
D) Parent Interviews: Doctors talk to parents about:
E) Observation through Play: Sometimes, just watching how the child plays, reacts, or explores gives the best clues.
Global Developmental Delay is more common than many people think, especially in children under 5. It’s estimated that 1% to 3% of young children have GDD. That means in a preschool with 100 kids, at least one or two may have some form of global developmental delay.
In many cases, early signs are missed because people think “every child grows at their own pace.” While that’s partly true, delays in multiple areas that persist over time need attention. GDD is not the same as lifelong disability.
With support programs for parents, early therapy, and individualized help, many children with GDD go on to learn, grow, and lead fulfilling lives.
a) Early Intervention Therapy: This is where the magic starts—speech therapy, occupational therapy, physiotherapy, and special education are blended like puzzle pieces to help the child learn communication, motor skills, and self-help tasks. The earlier this starts, the better the brain can rewire. Developmental delay therapy for children is part of most early intervention programs.
b) Medical Support: If the delay is linked to other conditions like seizures or genetic syndromes, doctors may prescribe anti-epileptics or hormonal treatments based on individual needs. In some cases, genetic tests or developmental issues are recommended to guide diagnosis.
Involves using herbs and massages (like Abhyanga) to support brain nourishment and detoxification, with a focus on balancing doshas (energy systems).

Used to manage secondary symptoms like sleep troubles, irritability, or constipation in children with GDD. Remedies are mild and individualized, but scientific evidence remains mixed.

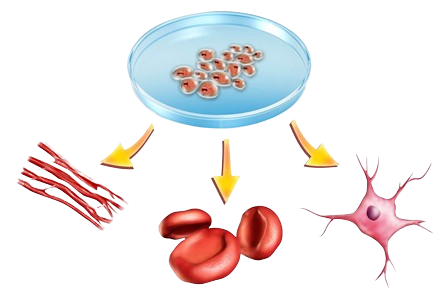
Still experimental, this method uses special cells believed to repair or calm the damaged areas in the brain. It’s done in controlled research settings only. It is being researched alongside stem cell therapy for autism.
In some cases, doctors try Hyperbaric Oxygen Therapy (HBOT) to increase oxygen to the brain, believed to help in neuroplasticity (the brain’s ability to adapt and grow). This overlaps with practices in autism rehabilitation centers.
Here, too, checking for gut imbalances, sleep hormones, and nutrition plays a role. Sometimes children labeled “delayed” begin making progress after addressing digestion and inflammation. It connects with growing interest in the gut microbiome and the gut-brain connection.

At Resplice Research Institute, doctors use a treatment called Gut Microbiota Transplantation (GMT) to help children with GDD, especially those who also struggle with stomach problems, sleep issues, irritability, and behavior challenges.
The big idea: Our gut (stomach and intestines) is filled with tiny living germs called bacteria, most of which help us digest food, keep our immune system strong, and even send signals to our brain. This is called the gut-brain connection. In many GDD children, these bacteria are not balanced—what we call gut dysbiosis—and that may affect how they feel, behave, or even think.
GMT works by transferring healthy bacteria from the poop of a healthy child (called a donor) into the gut of the GDD child. Over time, these new “good” bacteria settle into the child’s gut, help fix imbalances, and support better overall health.
A) Resplice Outcome in GDD:
What Makes GMT at Resplice Special? Here’s what makes the process safe, careful, and unique at Resplice:
1. Donor Screening with Global Standards:
Not just anyone can be a donor. At Resplice, donor screening is done using a set of international medical guidelines (called the International Stool Banking Consensus) and gut microbiome test. This includes:
2. Why Donors Are Kids, Not Adults:
Unlike other places that use adult donors, Resplice uses donors under age 12. Why?
3. Collection & Transport – Very Hygienic Process:
Every day, fresh stool is collected from the child donor in a germ-free, gamma-sterilized container (which means it’s super clean). Here’s how it’s handled:
The treatment isn’t done just once—multiple infusions are given over weeks to slowly reshape the gut-brain axis or the communication between gut and brain. Why? Because it takes time for the new bacteria to settle in, multiply, and take over the unhealthy ones in the child’s gut. Gradually, this reshapes the entire gut microbiome, which can lead to:
GMT is not about changing who someone is. It’s about helping the body and brain work together more smoothly by fixing what’s going on in the gut. At Resplice, this is done scientifically, safely, and with compassion, always as part of a bigger plan that includes therapy, nutrition, and emotional support.
GDD is when a child is growing, but at a slower rhythm across multiple areas—like walking, talking, thinking, or playing. Imagine a flower that blooms in late spring instead of early—still beautiful, just on its own timeline. With the right care and sunlight (therapy and support), it can flourish.
GDD means delays in two or more developmental areas. If a child struggles only with speech but moves and plays typically, it’s a single delay. GDD is more like several puzzle pieces taking longer to click into place—like speech + motor skills + learning—all needing gentle attention.
You might see your child not sitting up by 9 months, not speaking words by 2 years, not responding to their name, or needing help with tasks like dressing or eating beyond the expected age. These are like little flags—not warnings, but signals to check in.
No. GDD is a broad term used in children under 5 when it’s too early to give a more specific diagnosis. Some kids with GDD catch up fully; others may later be diagnosed with autism, intellectual disability, or a genetic condition. GDD gives us time to observe and support.
Absolutely not. GDD can be caused by many things—genetics, birth complications, infections, nutrition issues, or sometimes unknown factors. You didn’t cause this. What matters most is what you do now—early support makes a world of difference.
Sometimes, yes. Some children catch up fully, especially if the delay is mild and they receive early help. Others may continue to need support. Early intervention gives the brain a head start, helping it rewire before age 5, when it’s most flexible.
Doctors look at milestones, observe how your child plays, ask you detailed questions, and may recommend developmental screening tests, brain scans, or genetic testing. It’s a team effort involving pediatricians, therapists, and sometimes psychologists.
It depends on the child’s delays. Common ones include:
Speech therapy for talking and understandingSpecial education for learning skills
Therapies are like daily vitamins for the brain—small but powerful over time.
Not directly. But if your child has related issues like seizures, thyroid imbalance, or ADHD, medications may be prescribed to support those. Most of GDD treatment is therapy- and nutrition-based, not pharmaceutical.
A healthy gut supports a healthy brain. Children with GDD often have gut imbalances—like constipation, bloating, or picky eating—that affect mood, sleep, and focus. Fixing the gut can calm the brain, improve behavior, and make therapy more effective.
GMT gently replaces unhealthy gut bacteria with healthy ones from a carefully screened child donor. At Resplice, this is done through safe, clean infusions to rebalance the gut and boost the brain’s wiring. Many children show calmer moods, better sleep, and improved engagement after GMT.
At Resplice, only donors under age 12 are used (for their clean, natural microbiome), and every sample is rigorously screened. The process is done in sterile conditions with care and compassion. It’s not for every child—but for some, it can be a game-changer alongside therapy.
Some families explore:
Homeopathy for sleep or behaviorFunctional medicine to address nutrient gaps or toxins
These are best seen as complementary—not standalone—support systems.
GDD affects 1–3% of children under 5. Many signs are missed or explained away as “late blooming.” But GDD is more than slow growth—it’s a sign to support now, not wait. When caught early, many children go on to lead independent and joyful lives.
Start early, stay curious, and never compare your child’s journey to others. Trust your instincts. Therapy, gut care, and emotional connection together form the tripod that helps your child rise. Your love—and timely action—are the most powerful medicines.

Resplice Institute is India’s first integrated center offering autism therapy, gut microbiome treatment, and preventive health planning. We combine science and empathy to heal lives from the root.
© 2025 respliceinstitute.com || All Rights Reserved