- +91 91000 65552
- +91 9324982134
- contact@respliceinstitute.com
- Mon-sat 10:00 -18:00
Imagine your stomach and intestines as a busy train station. The trains (food) are supposed to pass through smoothly on schedule. But in Irritable Bowel Syndrome (IBS), the trains either rush too fast (causing diarrhea), crawl slowly (causing constipation), or stop randomly and make everyone uncomfortable (causing gas, pain, or bloating).
IBS isn’t like a broken bone that can be seen in an X-ray. It’s a functional disorder, which means the system doesn’t work right, but nothing shows up as damaged. It’s your gut miscommunicating with your brain. This misunderstanding causes the bowel to overreact to things like stress, certain foods, or even hormones.
IBS doesn’t cause permanent harm or increase cancer risk. But it can really mess with daily life. That’s why it’s one of the most commonly talked-about conditions in gut-brain research and gastrointestinal problems.

There isn’t just one version of IBS. It’s more like different moods of the same gut:

The intestines move too fast. You feel urgency, loose stools, and stomach cramps. Example: You eat something mild and find yourself rushing to the toilet multiple times a day.

The intestines move too slowly. You feel bloated, uncomfortable, and like nothing is "moving." Example: Even with fiber, you might go for days without relief.

Some days, it’s constipation. Other days, diarrhea. And no clear reason why. Example: It’s like the weather in your stomach keeps changing without warning.
These different types help doctors figure out the treatment for irritable bowel syndrome that suits your body best.
Here’s how it usually shows up:




These aren’t “just tummy issues.” IBS often comes with mood swings, irritability, and a sense that something’s always off. That’s why it’s being explored more in gut-brain connection and gut microbiome studies.
There’s no one villain behind IBS—it’s more like a team of tricky suspects working together:
Your brain and gut constantly talk to each other. When that communication is off, your gut may overreact. This is a central idea in the autism gut-brain axis, too.

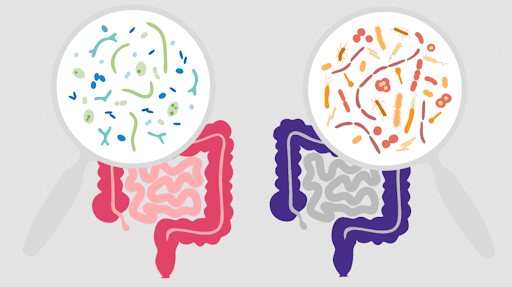
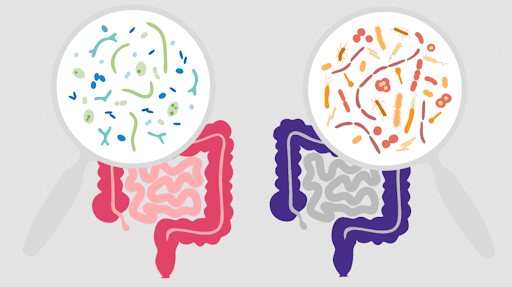
That’s when the “good” bacteria in your gut are outnumbered by the “bad” ones. Gut dysbiosis can trigger bloating, pain, and even affect mood.
IBS often worsens with anxiety, nervousness, or tension. Some even call the gut a "second brain."

Spicy foods, dairy, gluten, caffeine, and fried food are common triggers. But it’s different for each person.

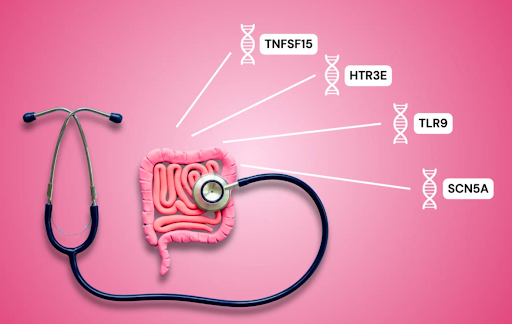
If a family member has IBS, or if you had a tough gut infection before, your chances go up.
Your brain and gut constantly talk to each other. When that communication is off, your gut may overreact. This is a central idea in the autism gut-brain axis, too.

That’s when the “good” bacteria in your gut are outnumbered by the “bad” ones. Gut dysbiosis can trigger bloating, pain, and even affect mood.
IBS often worsens with anxiety, nervousness, or tension. Some even call the gut a "second brain."

Spicy foods, dairy, gluten, caffeine, and fried food are common triggers. But it’s different for each person.

If a family member has IBS, or if you had a tough gut infection before, your chances go up.
There’s no one test to say “yes, this is IBS.” Doctors figure it out by ruling out other problems.
They’ll ask about symptoms, triggers, and patterns—especially if it’s lasted more than 3 months.

These help rule out infections, celiac disease, or inflammation (like in Crohn’s disease).

Only used if symptoms are serious or if there are red flags like weight loss or bleeding.

Sometimes doctors recommend a gut microbiome test to look at bacterial balance, especially when exploring gut issues in autism or functional gut disorders.
IBS affects about 10–15% of people worldwide. That’s more than 1 in every 10 people.
It’s more common in:
In places like India, IBS often goes undiagnosed or mislabelled as “gas trouble” or “stress.” But awareness is growing, especially with the popularity of gut microbiome research and FMT for irritable bowel syndrome.
IBS doesn’t show up in scans or leave scars, but it changes how you eat, sleep, study, and even socialize. It whispers through the gut, sometimes screams. But the more you listen, learn, and treat it with care, the more peace your body—and your brain—can find.
At Resplice Research Institute, doctors are using Gut Microbiota Transplantation (GMT) to help people with Irritable Bowel Syndrome (IBS)—especially those who deal with stubborn constipation, unpredictable diarrhea, painful bloating, gas, and brain fog that often comes with it.
The Big Idea: Fix the Gut, Calm the Storm
Think of your gut like a city full of tiny workers, bacteria that help digest food, manage inflammation, and even send messages to your brain about how you feel. In people with IBS, this city is often out of balance. Some of the workers have gone rogue, and the good ones aren’t strong enough to keep the peace. This is called gut dysbiosis, and it plays a huge role in how IBS symptoms appear and persist.
GMT works by gently introducing helpful bacteria from the poop of a healthy child (called a donor) into the gut of the person with IBS. It’s like replanting a garden: you remove the weeds, bring in fresh soil, and let new life grow. Over time, these “good” microbes settle in, crowd out the harmful ones, and bring the gut back into balance.
Resplice Outcome in IBS:
What Makes GMT at Resplice Different and Safe?
It doesn’t turn your gut into someone else’s—it simply helps your own body return to its natural rhythm by rebalancing what went wrong inside.
At Resplice, GMT for IBS is backed by science, handled with compassion, and always paired with diet advice, emotional support, and therapies as part of a bigger healing plan. It’s not about replacing medicines, but about giving your gut the support it needs to find peace again.
IBS is a common gut disorder where your stomach and intestines don’t work quite right. It causes cramping, bloating, gas, diarrhea, or constipation. It’s not dangerous, but it can be disruptive and uncomfortable.
IBS doesn’t damage the gut like ulcers or Crohn’s disease. It’s a functional problem—your gut miscommunicates with your brain, so symptoms happen even when tests come back normal.
There are three types:
IBS-D: Mostly diarrheaIBS-M: Mixed pattern of both
Knowing your type helps doctors tailor your treatment.
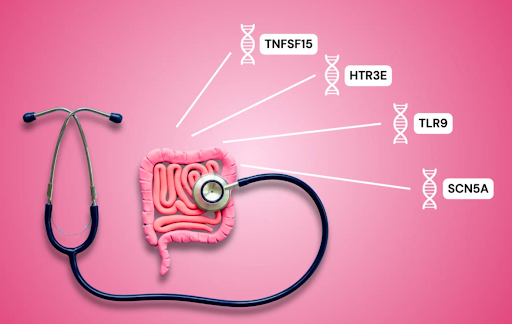
IBS can be caused by a mix of things: poor gut-brain communication, stress, gut dysbiosis (imbalance in gut bacteria), food triggers, past infections, or even genetics. Often, no single cause can be pinpointed.
Symptoms include gas, bloating, stomach cramps, irregular bowel movements (too often or not enough), mucus in stools, fatigue, and sometimes brain fog or anxiety.
Yes. IBS is closely connected to stress, anxiety, and emotions via the gut-brain axis. Emotional changes can worsen IBS symptoms and vice versa.
There’s no single test. Doctors use your history, rule out other diseases, and sometimes order stool tests, blood work, or a colonoscopy if needed.
There’s no one-time cure, but many people manage it well with a mix of diet changes, stress management, therapy, and—in some cases—microbiome-based treatments like GMT.
Common triggers include dairy, gluten, fried foods, caffeine, spicy meals, and artificial sweeteners. But it’s different for everyone. Keeping a food diary helps identify your personal triggers.
GMT involves transferring healthy bacteria from a child donor’s stool into the IBS patient’s gut. At Resplice, this helps restore microbial balance, calm symptoms, and support gut-brain communication.
Child donors have cleaner, less polluted microbiomes. Their gut bacteria are closer to nature, with fewer chemical exposures. This makes the transplant gentler and potentially more effective.
At Resplice, yes. They follow international screening standards, use sterile containers, test for infections, and use a cold-processing method to preserve good bacteria. Only the safest, cleanest samples are used.
GMT is done over several sessions. It’s not a one-time fix—it takes weeks for the new gut bacteria to settle and start changing the IBS symptoms. Most patients notice gradual improvement.
Beyond GMT, IBS management may include Ayurveda, homeopathy, probiotics, biofeedback, functional medicine, and gut-brain therapy. Each works differently, and many people combine them for the best outcome.
Yes. Children with autism often show signs of IBS or gut sensitivity. Therapies like GMT and gut-brain axis treatment are used in both IBS and autism-related care at places like Resplice.

Resplice Institute is India’s first integrated center offering autism therapy, gut microbiome treatment, and preventive health planning. We combine science and empathy to heal lives from the root.
© 2025 respliceinstitute.com || All Rights Reserved