- +91 91000 65552
- +91 92810 19252
- contact@respliceinstitute.com
- Mon-sat 10:00 -18:00
ADHD stands for Attention-Deficit/Hyperactivity Disorder. It’s a condition where the brain finds it tough to filter distractions, sit still, or control impulses, especially in situations where focus is expected. It is one of the conditions that often overlaps with or is seen alongside autism spectrum disorders, though they are different.
Think of your brain like a TV remote. Most people can press play, pause, or rewind their thoughts to some extent. But someone with ADHD has a glitchy remote—suddenly flipping channels, skipping buttons, switching to random programs—even when they want to watch just one.
Imagine sitting in class and trying to listen, but your brain is zipping through thoughts: “Did I bring my notebook? That fan is loud. I’m hungry. Is it lunch yet? What did the teacher just say?” You’re trying. Really. But your brain just won’t settle.

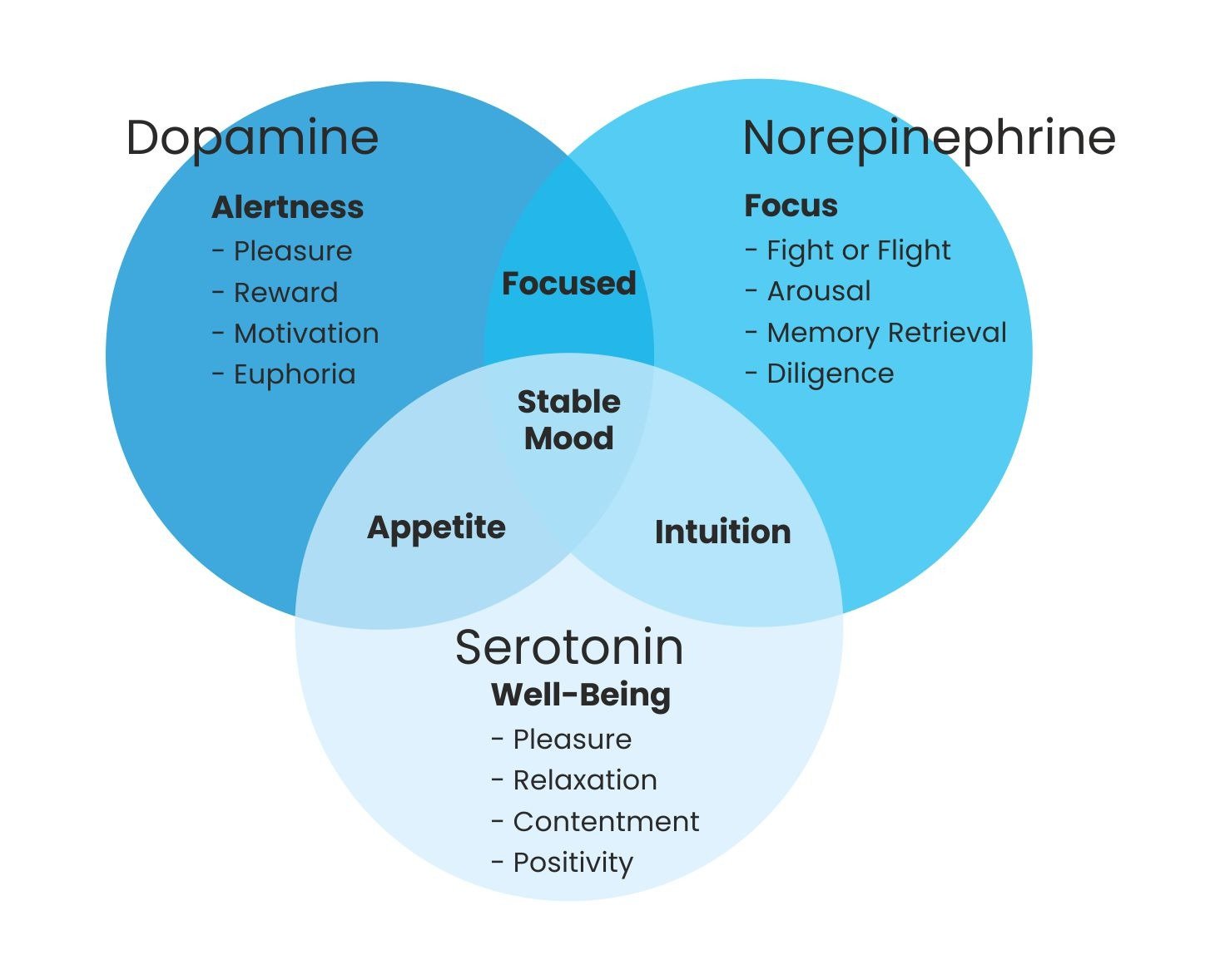
ADHD isn’t about being lazy or not smart. It’s linked to brain chemicals that help with alertness and attention—dopamine and norepinephrine. These chemicals don’t flow smoothly in ADHD brains, so it becomes harder to stay focused, stay motivated, or stay still.
Many with ADHD are highly creative, sharp thinkers. The difference is in how their brain is wired. That affects how they learn, behave, and even interact with people. With the right support, including treatment for ADHD that fits the child’s needs, the struggles can be managed, and strengths can shine.
ADHD doesn’t look the same in everyone. Doctors group it into three main types, based on the strongest symptoms.
Inattentive Type (this used to be called attention-deficit disorder – ADD): This type is about zoning out. The common signs are:
E.g. – You’re supposed to do math homework, but 20 minutes later, you’ve drawn five pages of doodles and your math page is still blank.
This type shows up more in how your body moves and how quickly you act without thinking.
E.g. – You’re sitting in class but you’re tapping your foot, bouncing your leg, and suddenly saying something out loud that was going on in your mind before realizing you’ve interrupted.
Most teens fall under this group—it’s a mix of both types-restless energy, drifting focus, impulsive decisions all bundled into one. Cognitive behavioral therapy for kids may help with regulating thoughts and emotions in such cases.
Imagine your brain has 50 tabs open—all flashing alerts. That’s what a regular day might feel like for someone with ADHD. ADHD signs usually start before age 12 and show up in more than one setting—home, school, or with friends.
You think you've been scrolling on your phone or reading a story or playing with building blocks for 10 minutes. It’s been 2 hours.
You think you've been scrolling on your phone or reading a story or playing with building blocks for 10 minutes. It’s been 2 hours.
You’re laughing one second, furious the next. Small things can feel like big storms.
The body is tired, but the brain's still doing somersaults at midnight.
You think you've been scrolling on your phone or reading a story or playing with building blocks for 10 minutes. It’s been 2 hours.
You think you've been scrolling on your phone or reading a story or playing with building blocks for 10 minutes. It’s been 2 hours.
You’re laughing one second, furious the next. Small things can feel like big storms.
The body is tired, but the brain's still doing somersaults at midnight.
First, let’s look at what DOESN’T cause ADHD:
These are myths. ADHD is real, and blaming the child (or the parents) helps no one. There’s no single reason why ADHD happens. Science points to a mix of genetics, brain structure, and early life influences such as:
Things like being born early, low birth weight, or exposure to smoking or alcohol during pregnancy can increase ADHD risk.
Toxins like lead or too much screen time may play a small role, but they’re not direct causes. Some clinics that follow functional medicine approaches may test for such factors.
The parts of the brain that help with focus, planning, and control may work differently or develop more slowly. Brain scans even show differences in ADHD brains, especially in areas like the prefrontal cortex that manage attention and control.
If your parent or sibling has ADHD, chances are higher that you might too. It often runs in families. For some children, a genetic test for autism or ADHD may be offered to explore inherited traits.
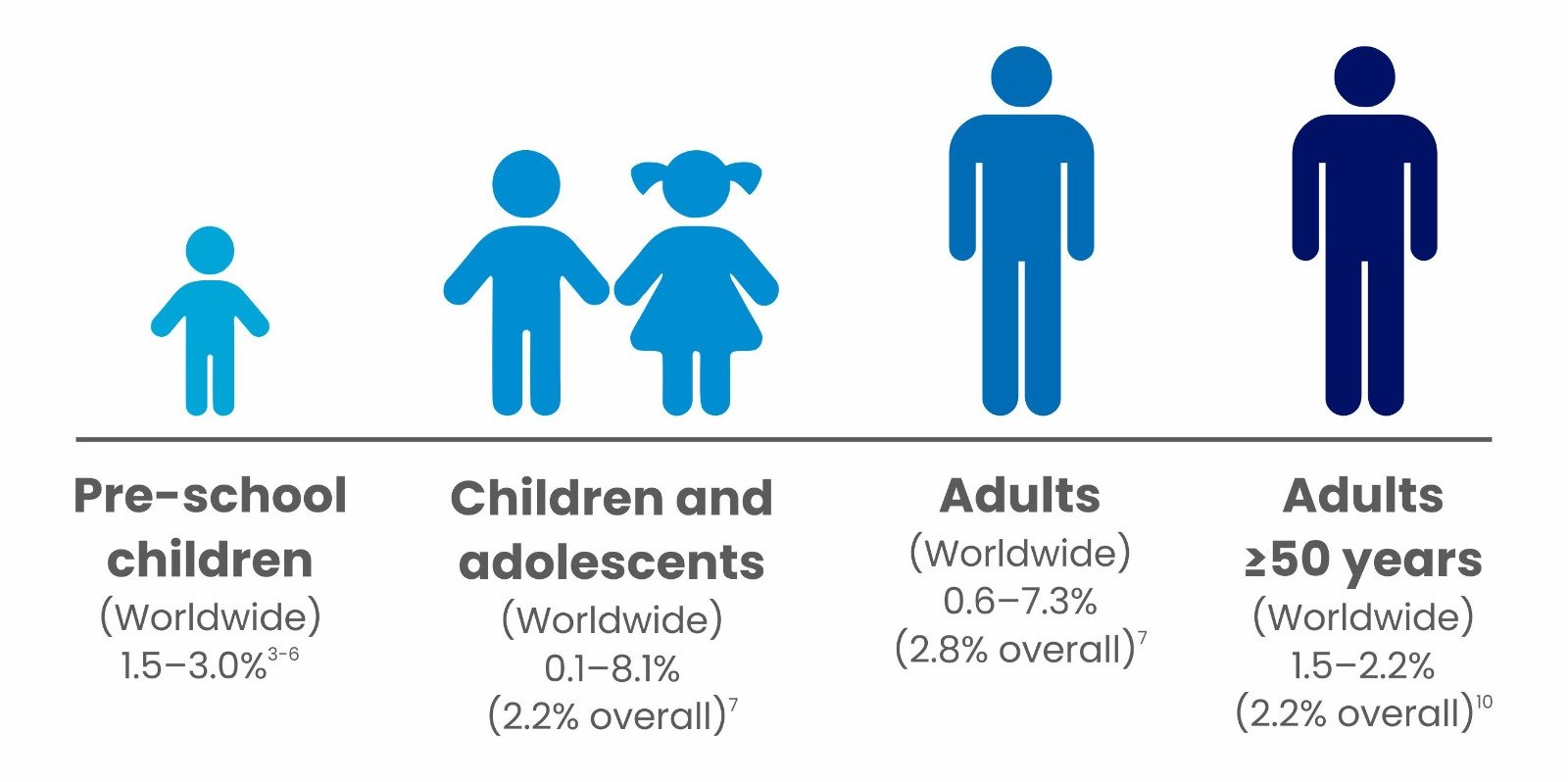
ADHD is one of the most common conditions among kids and teens. In a classroom of 30 students, one or two probably have ADHD, but each one will show it differently.
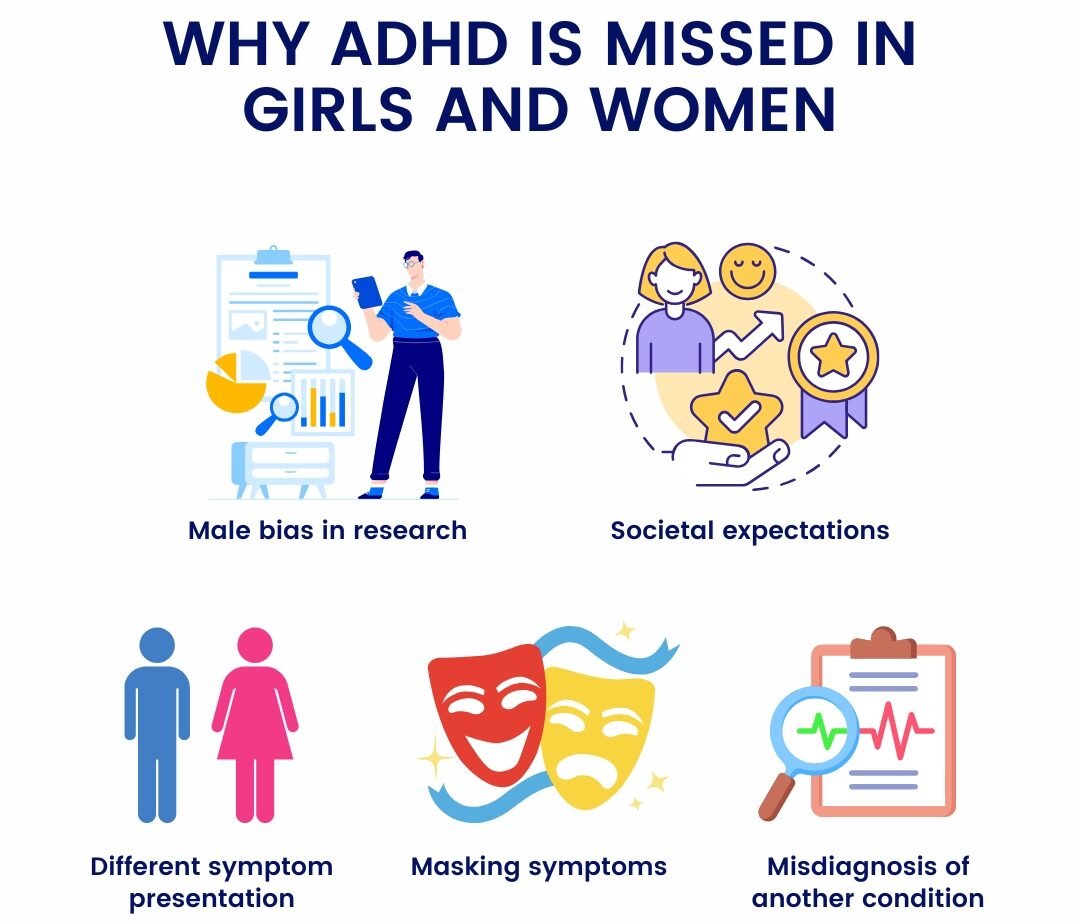
Why girls often go undiagnosed:
ADHD doesn’t go away in adulthood. About 60–70% of kids with ADHD continue to have symptoms as adults, but the challenges shift. Adults with ADHD may face:
Adults looking for support often turn to pediatric counseling services when their struggles are first recognized through their children.
There’s no “blood test” for ADHD. Diagnosis is done by observing, asking questions, and ruling out other issues.
Doctors talk to the child and the family. Teachers may also be asked to share their observations. You might fill out rating scales that ask things like:
Sometimes, poor hearing, vision problems, anxiety, or learning issues can look like ADHD. So doctors check for these too, often at a certified autism therapist or pediatric behavioral clinic.
Some clinics use computer tests to see how long you can focus or how quickly you react to things. It’s not about right or wrong—it’s about how your brain works.
ADHD doesn’t mean you’re broken. It just means your brain runs on a different frequency—sometimes fast, sometimes all over the place. But with the right tools, therapy, maybe medication, and support from people who get it, you can build a life that works for your brain, not against it.
Whether through early intervention programs, child psychology services, or even community-based ADHD treatment centers, what matters most is that no one has to go through it alone.
Behavioral Therapy & Special Education: ADHD is often managed through structured routines, reward systems, and one-on-one strategies. Think of it like giving your brain a daily workout plan—breaking big tasks into smaller ones, using timers, charts, and consistent feedback. In school, teachers may offer seating adjustments, extra breaks, or visual cues to help a child stay focused. This is a major component of behaviour therapy and is often supported in special education services offered at child development centers or inclusive schools.
Medical Management: Medications don’t “fix” ADHD, but they help calm the noise inside the brain. These include stimulants like methylphenidate, which boost dopamine and norepinephrine, the chemicals that help with attention and impulse control. It’s like adjusting the volume on a speaker so you can finally hear the right tune. Such options fall under treatment for ADHD and are often part of pediatric therapy services in structured centers.
1 . Homeopathy & Ayurveda:
Some families explore homeopathic drops or Ayurvedic herbs believed to balance energy, improve digestion, or reduce restlessness. These systems aim to address the child as a whole, not just the behavior. However, results vary widely, and these should always be used with guidance, not as a substitute for mainstream care.
2 . Functional Medicine:
Some doctors run deep tests to check for gut issues, food sensitivities, or nutrient deficiencies—things that might not cause ADHD but can worsen it. A tailored diet, sleep support, and probiotics are then used to regulate energy, mood, and attention. In some centers offering child psychology services or autism spectrum disorder therapy, functional medicine is paired with behavioral plans.
3 . Neurofeedback (Biofeedback):
A child wears a headband with sensors while watching a cartoon. When their brain stays calm or focused, the cartoon plays smoothly. When it doesn’t, the screen freezes. Over time, the brain learns to stay in that “focused” state longer. It’s like brain-training through gaming. This emerging field overlaps with cognitive behavioral therapy for kids and social skills training for children.
At Resplice Research Institute, doctors use a treatment called Gut Microbiota Transplantation (GMT) to help children with ADHD, especially those who also struggle with stomach problems, sleep issues, irritability, and behavior challenges.
The big idea: Our gut (stomach and intestines) is filled with tiny living germs called bacteria, most of which help us digest food, keep our immune system strong, and even send signals to our brain. This is called the gut-brain connection. In many adhd children, these bacteria are not balanced—what we call gut dysbiosis—and that may affect how they feel, behave, or even think.
GMT works by transferring healthy bacteria from the poop of a healthy child (called a donor) into the gut of the adhd child. Over time, these new “good” bacteria settle into the child’s gut, help fix imbalances, and support better overall health.
Resplice Outcome in ADHD:
What Makes GMT at Resplice Special? Here’s what makes the process safe, careful, and unique at Resplice:
1 . Donor Screening with Global Standards:
Not just anyone can be a donor. At Resplice, donor screening is done using a set of international medical guidelines (called the International Stool Banking Consensus) and gut microbiome test. This includes:
2 . Why Donors Are Kids, Not Adults:
Unlike other places that use adult donors, Resplice uses donors under age 12. Why?
3 . Collection & Transport – Very Hygienic Process:
Every day, fresh stool is collected from the child donor in a germ-free, gamma-sterilized container (which means it’s super clean). Here’s how it’s handled:
4 . It’s a Process, Not a One-Time Thing:
The treatment isn’t done just once—multiple infusions are given over weeks to slowly reshape the gut-brain axis or the communication between gut and brain. Why? Because it takes time for the new bacteria to settle in, multiply, and take over the unhealthy ones in the child’s gut. Gradually, this reshapes the entire gut microbiome, which can lead to:
GMT is not about changing who someone is. It’s about helping the body and brain work together more smoothly by fixing what’s going on in the gut. At Resplice, this is done scientifically, safely, and with compassion, always as part of a bigger plan that includes therapy, nutrition, and emotional support.
Not at all. ADHD is not about bad behavior—it’s about a brain that processes the world differently. It may look like restlessness or forgetfulness on the outside, but inside, it's a storm of noise, distraction, and emotion all happening at once.
Yes. Some children, especially girls, may seem dreamy or overly quiet. This is called inattentive ADHD. They may miss instructions, lose track of time, or forget what they were saying mid-sentence—but they’re not trying to be lazy.
ADHD is not caused by too much sugar, screen time, or bad parenting. It's a neurodevelopmental condition influenced by genetics, brain chemistry, and sometimes early life factors like birth trauma or inflammation.
Because ADHD is not a constant deficit—it’s an inconsistency of control. Think of it like a flickering light. When it shines, your child may appear focused. When it dims, they may seem lost. It's not willful—it’s neurological.
Diagnosis involves interviews, checklists, observations, and sometimes school reports. It’s not based on one test, but a pattern of behaviors over time. A trained professional—psychologist, psychiatrist, or developmental pediatrician—usually does this.
Their thoughts race like wildfire—blazing faster than social rules can catch up. They don’t mean to be rude. Their brain is just sprinting through ideas, and the words tumble out before the brakes can hit.
Yes. Many children with ADHD have trouble falling asleep, staying asleep, or feeling rested. They may also have tummy troubles—constipation, food sensitivities, or gut-related mood swings. That’s where gut-brain therapies like GMT come in.
GMT involves transferring healthy gut bacteria from a screened child donor into your child’s intestine, aiming to reset the gut ecosystem. For children with ADHD and gut imbalances, this may support better focus, mood regulation, and digestion.
Very. ADHD rarely travels alone. Anxiety, sensory sensitivities, or learning difficulties often tag along. It’s not your fault—it’s just that when the brain struggles to filter input, emotions often overflow.
Therapy helps immensely. Occupational therapy, behavior therapy, social-emotional coaching, and parent training can help children develop skills, regulate emotions, and feel more understood. Medicine is a tool—not the whole toolbox.
That’s a personal decision. Some children thrive with medicine; others manage well with therapy alone. If you do choose medication, a qualified doctor will guide the dosage, monitor side effects, and adjust as your child grows.
Because intelligence and executive function are not the same. Your child might understand complex ideas but struggle to start tasks, manage time, or finish homework. Think of it like having a brilliant mind trapped behind a foggy windshield.
ADHD often continues into adolescence and adulthood, but it evolves. With support, many children learn to work with their brain’s rhythm—turning chaos into creativity, and distraction into discovery.
Absolutely. Girls often go undiagnosed because they internalize their struggles. They may be praised for being "well-behaved" while silently battling anxiety, overthinking, or sensory overload. Quiet doesn’t mean unaffected.
Believe your child. Listen beyond the behavior. Advocate when others don’t understand. ADHD isn’t a flaw—it’s a different frequency. And with the right environment, that frequency can sing.

Resplice Institute is India’s first integrated center offering autism therapy, gut microbiome treatment, and preventive health planning. We combine science and empathy to heal lives from the root.
© 2025 respliceinstitute.com || All Rights Reserved