- +91 91000 65552
- +91 9324982134
- contact@respliceinstitute.com
- Mon-sat 10:00 -18:00
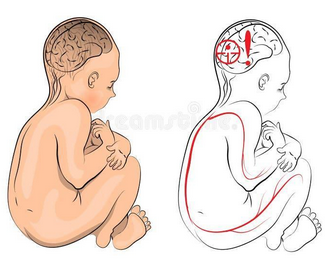
Cerebral Palsy (CP) is a condition that affects a person’s movement, muscle strength, and body coordination. It happens when there is a problem with the way the brain develops or works, especially the part that controls how our body moves.
Let’s imagine your brain as the Remote of a TV, and your muscles are the different functions like volume, brightness, etc. The brain sends out commands through signals (nerves) to tell your arms, legs, and body what to do. In CP, those signals get scrambled, delayed, or misdirected—so the body doesn’t move smoothly.
It’s called “cerebral” because it starts in the brain, and “palsy” because it affects posture and movement. CP is not a disease, and it doesn’t get worse over time. But the challenges it causes can change as a person grows.
CP usually appears in the first few years of life, and affects each child differently—some may have slight issues with balance or coordination, while others may need support with walking, sitting, or talking.
There are four main types of Cerebral Palsy, depending on how the muscles are affected and how the person moves. Each one has its pattern.
There are different subtypes:
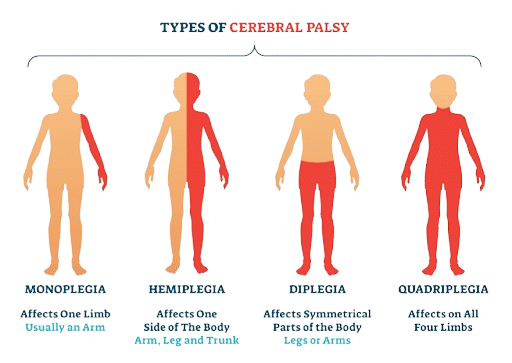
Apart from this, there is also

Each type requires a unique therapy approach, which may include pediatric therapy services like sensory, physical, or behavioral support.
The symptoms of CP vary depending on how severe the brain injury is and what part of the brain is affected. But most of the signs appear in infancy or early childhood.
Here’s what you might notice:
Some children with CP may also face learning difficulties, while others have average or above-average intelligence. CP doesn’t affect the mind directly, but challenges in movement and communication can sometimes make learning harder without support. This is why many families opt for special education services that adapt teaching strategies to a child’s motor and speech abilities.
Important note: In many cases, no exact cause is found, but it’s clear that the injury happened early on and did not come from anything the parents did or didn’t do. If the cause is unclear, doctors may recommend a genetic test for autism or CP-related conditions to rule out hereditary factors.
There’s no single test that says, “Yes, this is CP.” Doctors use a combination of observation, physical exams, and brain imaging to diagnose it.
Here’s how it usually works:
A) Developmental Observation: Doctors look for signs like delayed milestones, muscle stiffness, or unusual movement patterns, especially if the baby isn’t sitting or crawling at the expected time. This may be followed by developmental delay treatment if early signs are confirmed.
B) Physical & Neurological Exam: A pediatrician or neurologist checks:
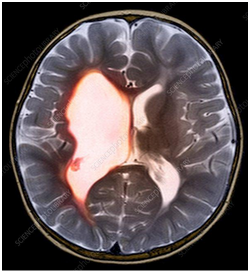
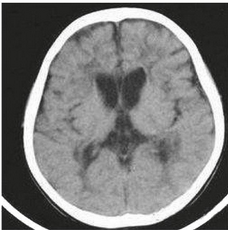
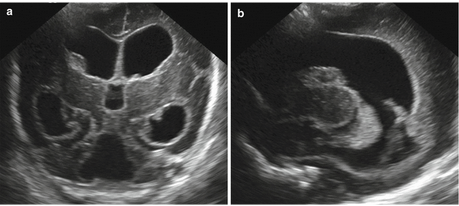
C) Brain Scans: These help doctors understand what kind of brain damage may have occurred.
D) Hearing and Vision Tests:
E) Other Assessments:
Diagnosis can take time, especially in babies with mild symptoms. But the earlier CP is identified, the sooner therapy can begin, and that makes a big difference. Most children benefit from starting with early intervention programs.
Cerebral Palsy is the most common motor disability in childhood. Around 2 to 3 children out of every 1,000 births are diagnosed with CP worldwide. That means in a large school, several students may be living with CP, each with very different needs and abilities. CP doesn’t get worse as the child grows, but their challenges can change. Some kids improve their movement with therapy and support. Others may need mobility aids or assistive technology as they grow older.
Children and teens with CP are just like anyone else—they have feelings, dreams, hobbies, and talents. What they need is understanding, encouragement, and the right kind of help to live life to the fullest. Support programs for parents or CP-specific networks can make a meaningful difference in their journey.
A) Neuro-Rehabilitation Therapy: This is the heart of CP management. It includes:
Think of it as tuning a musical instrument every day. The brain might send the wrong notes, but with practice, the body learns to play better. These are core parts of occupational therapy and speech therapy for children offered at specialized rehabilitation centres.
B) Medical Management: Doctors may use medicines like muscle relaxants (e.g. baclofen) or even Botox injections to reduce tightness in specific muscles. Anti-seizure drugs may be needed too.
Ayurveda uses therapies like Panchakarma detox, herbal oils, and diet modifications to reduce spasticity and improve calmness. Therapies like Shirodhara (pouring oil over the head) are used to relax the nervous system. Some autism treatment centers offer Ayurvedic-based care as part of integrative healing.

Given for associated issues—drooling, seizures, irritability—but not a replacement for therapies.

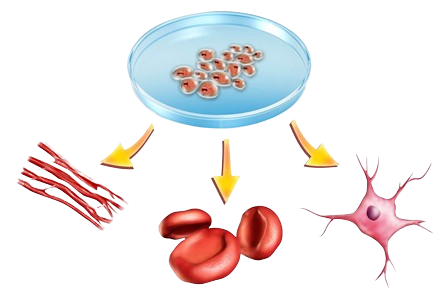
In CP, the idea is that stem cells can regenerate damaged areas in the brain or spinal cord. Early trials are ongoing, but it’s still under research. It overlaps with research in autism spectrum disorders.
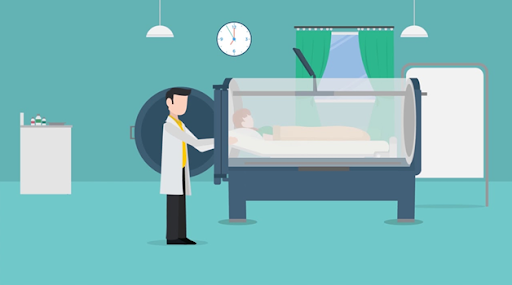
HBOT helps increase oxygen in the brain and body, which may improve mobility, alertness, or mood in some children. This has been explored in autism spectrum disorder treatment.
Advanced tools help children recognize when their muscles are too tight or too relaxed, and gently train them to regain control. It’s like giving the brain a “mirror” to understand how the body is reacting. These tools are part of pediatric therapy services and behavioral therapy for autism.

CP may not go away, but improving gut health, sleep quality, immunity, and inflammation can make day-to-day life smoother. A child with CP who is well-rested, calm, and digesting food well is more likely to benefit from therapy sessions. This ties in with growing interest in autism and gut health, gut-brain research, and gut dysbiosis.

At Resplice Research Institute, doctors use a treatment called Gut Microbiota Transplantation (GMT) to help children with CP, especially those who also struggle with stomach problems, sleep issues, irritability, and behavior challenges.
The big idea: Our gut (stomach and intestines) is filled with tiny living germs called bacteria, most of which help us digest food, keep our immune system strong, and even send signals to our brain. This is called the gut-brain connection. In many CP children, these bacteria are not balanced—what we call gut dysbiosis—and that may affect how they feel, behave, or even think.
GMT works by transferring healthy bacteria from the poop of a healthy child (called a donor) into the gut of the CP child. Over time, these new “good” bacteria settle into the child’s gut, help fix imbalances, and support better overall health.
a) Resplice Outcome in CP:
What Makes GMT at Resplice Special? Here’s what makes the process safe, careful, and unique at Resplice:
Not just anyone can be a donor. At Resplice, donor screening is done using a set of international medical guidelines (called the International Stool Banking Consensus) and gut microbiome test. This includes:
Unlike other places that use adult donors, Resplice uses donors under age 12. Why?
Every day, fresh stool is collected from the child donor in a germ-free, gamma-sterilized container (which means it’s super clean). Here’s how it’s handled:
The treatment isn’t done just once—multiple infusions are given over weeks to slowly reshape the gut-brain axis or the communication between gut and brain. Why? Because it takes time for the new bacteria to settle in, multiply, and take over the unhealthy ones in the child’s gut. Gradually, this reshapes the entire gut microbiome, which can lead to:
GMT is not about changing who someone is. It’s about helping the body and brain work together more smoothly by fixing what’s going on in the gut. At Resplice, this is done scientifically, safely, and with compassion, always as part of a bigger plan that includes therapy, nutrition, and emotional support.
Cerebral Palsy is a condition where the brain has trouble telling the body how to move. Imagine the brain as a remote control and the muscles as a TV—if the signals from the remote get scrambled, the channels (movements) won’t respond properly. That’s what happens in CP.
CP isn’t a disease, and it doesn’t "spread" or get worse. But as a child grows, their needs may change. Therapy and support can help them get stronger and more independent over time.
You might notice stiff or floppy muscles, delayed milestones like sitting or crawling, favoring one side of the body, or trouble with balance. Some children may also have difficulty swallowing, speaking, or show jerky movements.
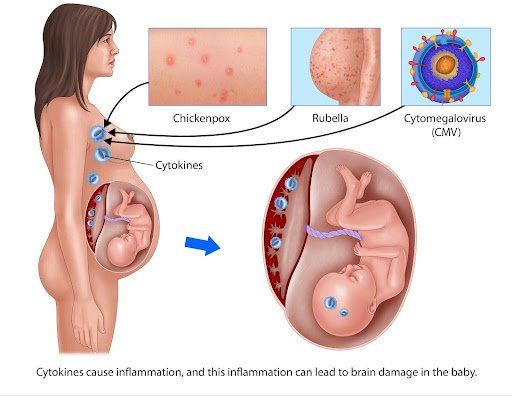
CP happens due to early brain injury—before, during, or after birth. This can be from infections, lack of oxygen, premature birth, or head injury. Sometimes, the exact cause remains unknown, and that’s okay—it’s not your fault.
CP mostly affects movement, but some children may face learning challenges—especially if their speech or motor skills make communication harder. Many children with CP have average or above-average intelligence.
Some can, and some may need extra help. Children with mild CP may walk independently; others may use walkers or wheelchairs. Speech therapy often supports communication, whether verbal or through alternative tools.
Therapy is the heart of CP care:
Physiotherapy strengthens musclesSpeech therapy helps with talking or swallowing
Think of it a
Yes. Doctors might use muscle relaxants, Botox for stiff areas, or anti-seizure medications. These aren’t cures, but tools to ease symptoms and make therapy more effective.
Some families explore Ayurveda, Homeopathy, Stem Cell Therapy, or Hyperbaric Oxygen Therapy (HBOT). While some show promise, always consult your doctor. These should complement, not replace, standard therapy.
Children with CP often struggle with digestion, mood, and sleep—all tied to the gut-brain connection. An unbalanced gut (called gut dysbiosis) can make everything from therapy to mood regulation harder.
GMT transfers healthy gut bacteria from a screened child donor to the child with CP. This can reset the gut environment, supporting better digestion, calmer behavior, improved sleep, and more responsive therapy sessions.
At Resplice, GMT is done with extreme care:
Donors are healthy children under 12, thoroughly screenedMultiple sessions help new bacteria settle in over time
It’s a scientific, step-by-step process backed by safety protocols.
Be their biggest encouragement. Advocate for therapies early, believe in their potential, and celebrate every small win. CP may change how a child moves—but not how deeply they can love, learn, or live.

Resplice Institute is India’s first integrated center offering autism therapy, gut microbiome treatment, and preventive health planning. We combine science and empathy to heal lives from the root.
© 2025 respliceinstitute.com || All Rights Reserved