- +91 91000 65552
- +91 9324982134
- contact@respliceinstitute.com
- Mon-sat 10:00 -18:00
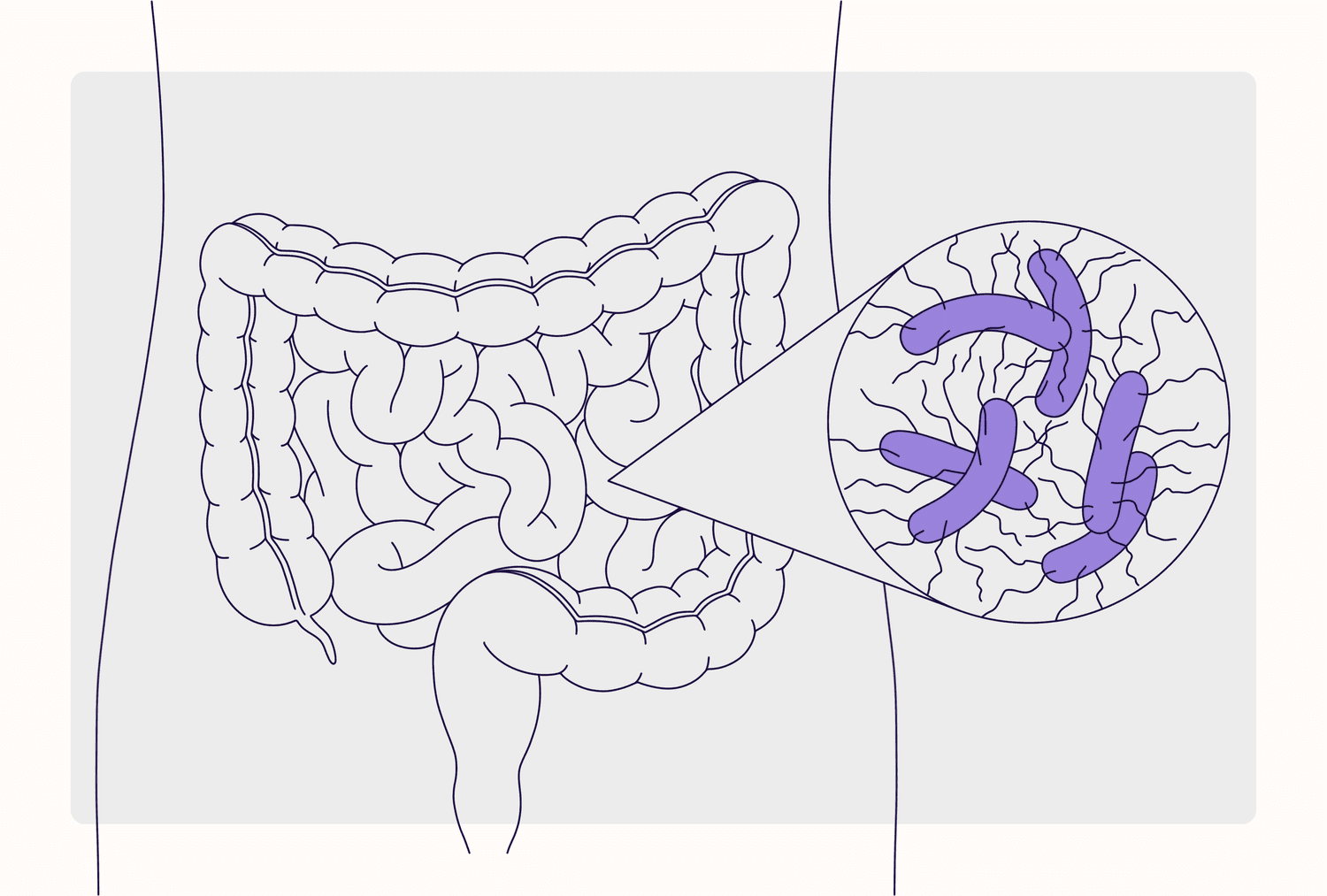
Clostridium difficile, or C. diff, is a type of bacteria that can live in the gut. Usually harmless, it can turn troublesome when antibiotics disturb the normal balance. Once it overgrows, it produces toxins that cause watery diarrhea, abdominal pain, fever, and sometimes more serious gut damage. This condition is called Clostridium difficile infection or CDI.
Think of your gut like a garden. Under normal care, flowers (good bacteria) and soil microbes coexist peacefully. But if you spray broad-spectrum antibiotics, many of the good flowers die. Suddenly, weeds—like C. diff—take hold and spread fast, choking the garden and causing chaos.
C. diff infections vary in severity and presentation:
Each type requires different levels of treatment, monitoring, and support.
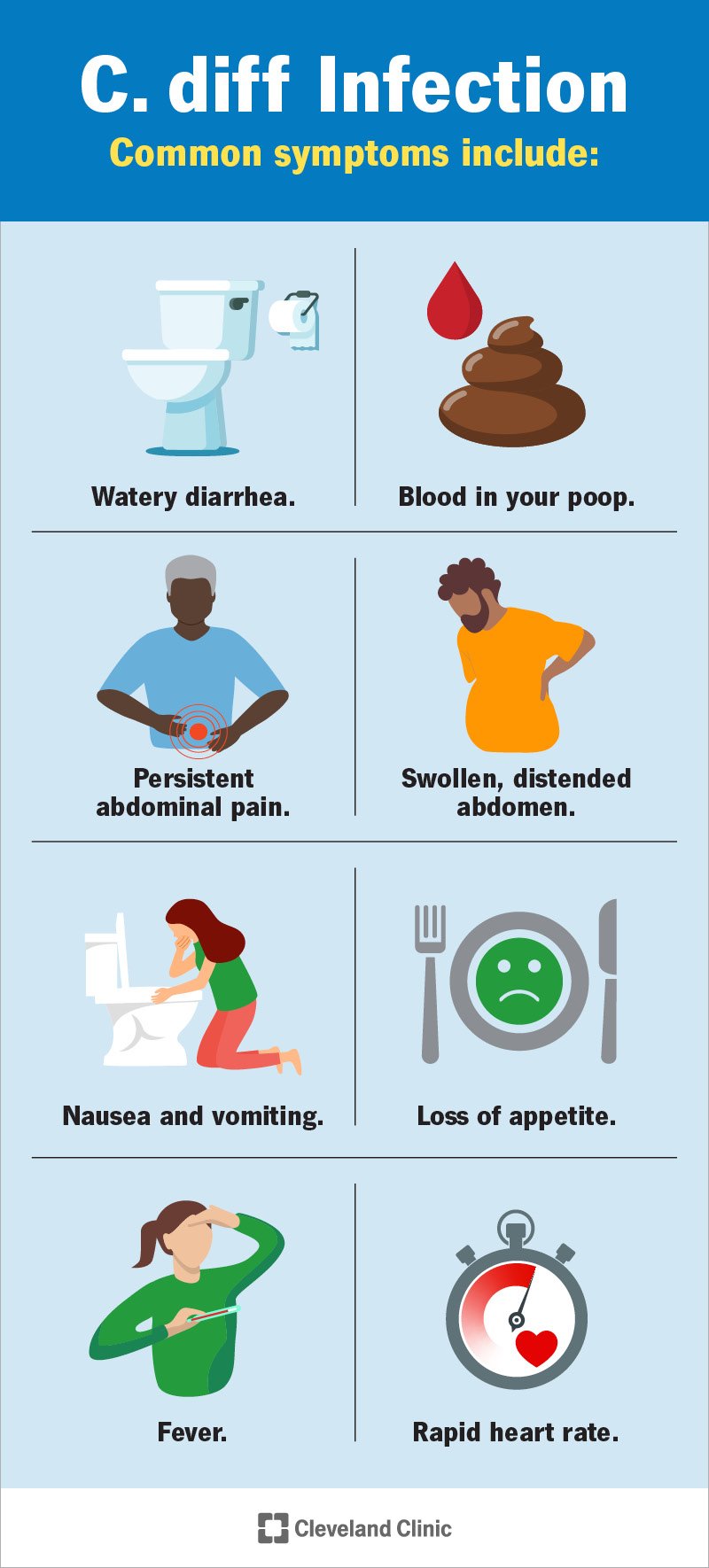
Symptoms typically appear 1–2 weeks after antibiotics, but can emerge sooner or even later.
Common signs include:
If you’re on antibiotics and experience these, it’s worth getting checked—even days after finishing the meds.
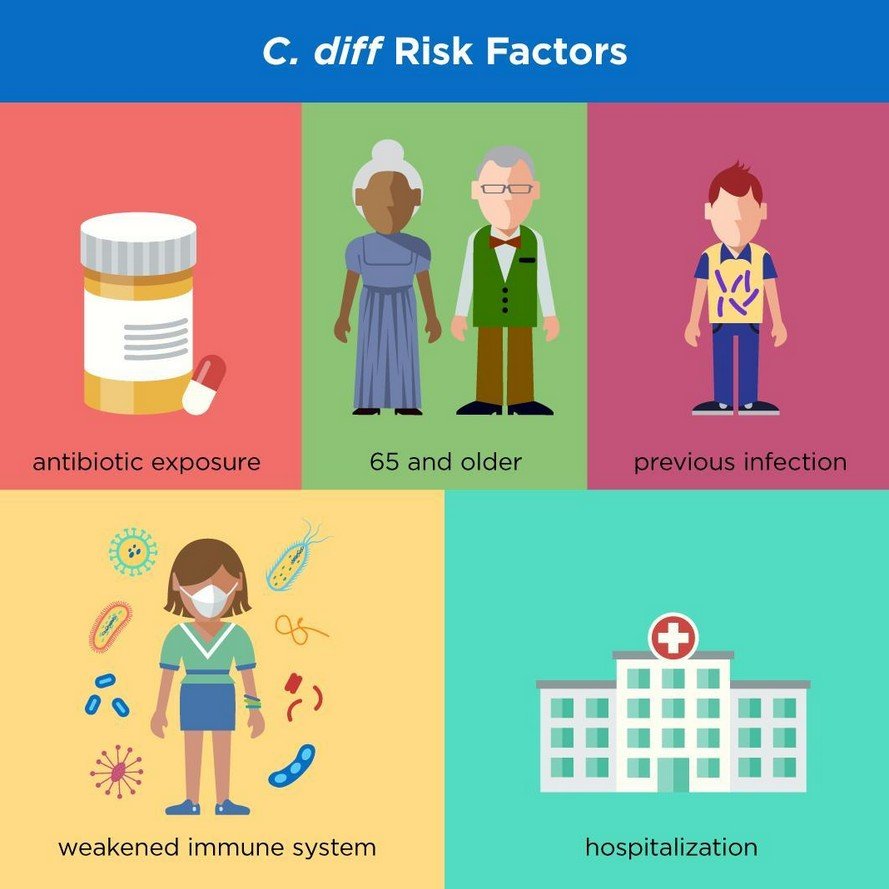
The main trigger is antibiotic use. Tablets like clindamycin, cephalosporins, or penicillin wipe out good bacteria, allowing C. diff to flourish.
Other risk factors:
Once the healthy gut bacteria are gone, C. diff can take over and produce toxins that damage the gut lining.

Diagnosing requires two things:
Common tests:
Sometimes imaging studies like CT scans are needed for severe cases to check for gut complications.

Globally, CDI rates are increasing—especially in healthcare settings where antibiotic protocols are still being strengthened.
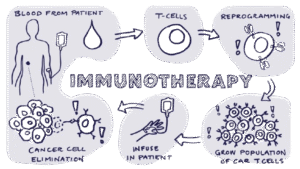
At Resplice, our GMT protocol for recurrent CDI is meticulously designed for both efficacy and safety—and deeply integrated into our philosophy of healing the whole person, not just the infection.
1. CDI often occurs when the gut ecosystem is stripped bare. That leaves gut dysbiosis, which allows C. diff to flourish. GMT reseeds the gut with rich, beneficial bacterial communities, essentially restoring the balance.
2. Clinical studies show success rates over 90% in recurrent CDI—dramatically higher than retreatment with antibiotics alone.
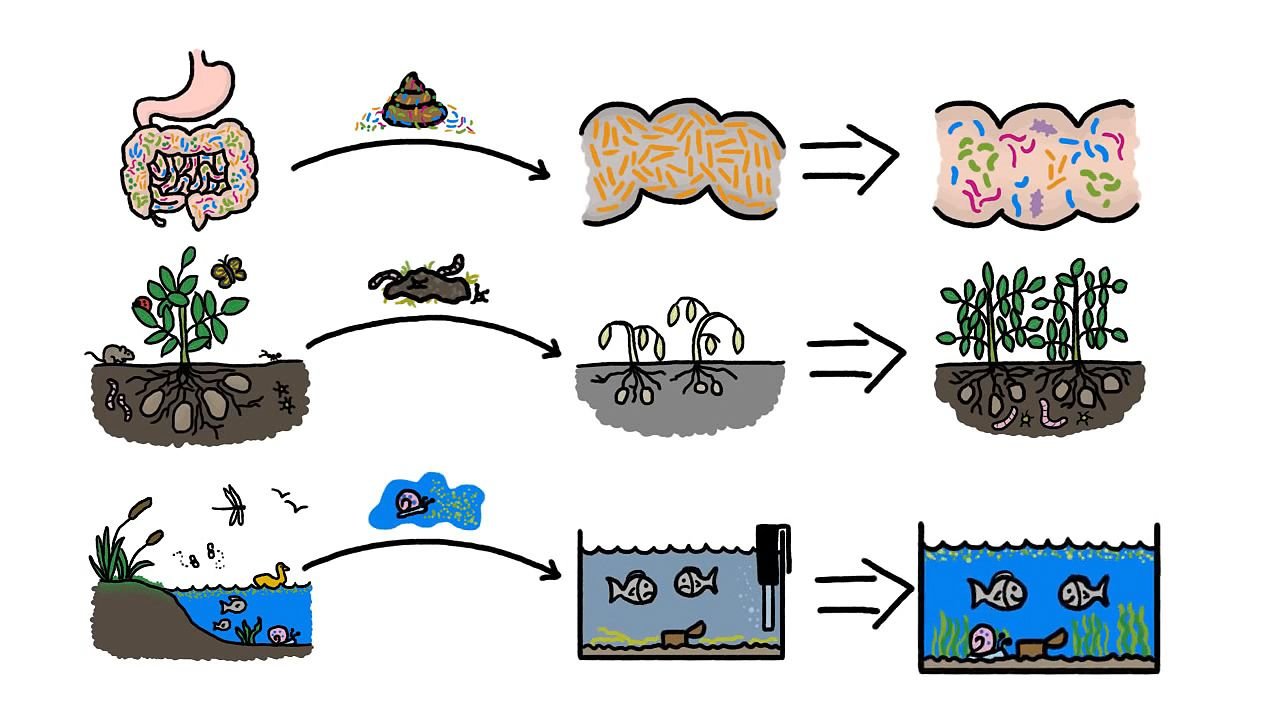
1. Child Donors Under 12: Strong microbiome, fewer accumulated toxins, and microbial patterns more similar to natural development.
2. International Screening Standards: All donors are tested against protocols like the International Stool Bank Consensus plus gut microbiome profiling and food intolerance panels. No shortcuts.
3. Sterile Processing in Laboratory Settings: Fresh stool is collected in gamma-sterilized containers, transported at 4 °C, blended, filtered, and centrifuged—only the purified liquid (supernatant) containing beneficial bacterial populations is used.
4. Multistep Colonic Infusion Protocol: Rather than one dose, patients receive multiple infusions over several days or weeks, gently allowing beneficial bacteria to engraft and re-establish a healthy microbiome.
5. Holistic Post-GMT Support: GMT is paired with dietary guidance (prebiotics, fiber), stress-reduction strategies, and optional supportive therapies like yoga, pranayama, or functional supplements.
Patients with multiple CDI recurrences not only stabilize their bowel habits but often report better energy, improved mood, and fewer gut-related anxieties. The treatment shifts focus from just “treating diarrhea” to restoring resilience and gut-brain harmony.
These are medically approved, evidence-based approaches that aim to eliminate the infection and stabilize the patient:
Vancomycin or fidaxomicin—target the Clostridium difficile infection directly. Think of them as specialized cleanup crews sent in to remove the weeds (toxic bacteria) from the garden (gut).

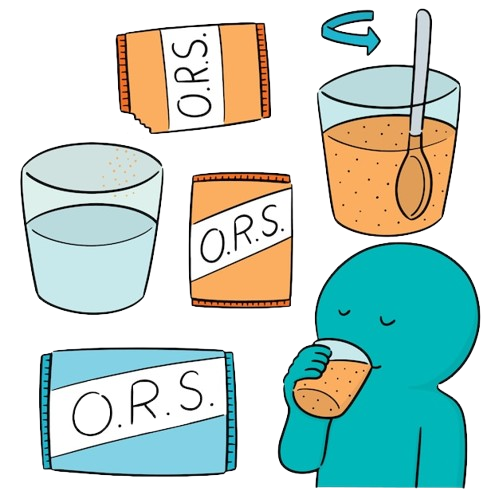
Frequent diarrhea can dehydrate and unbalance body chemistry—IV fluids or pediatric oral solutions help restore balance.
If possible, the antibiotic that sparked the CDI is stopped or switched.

While not strong enough alone for active infection, probiotics may help prevent recurrence when taken along with antibiotics.
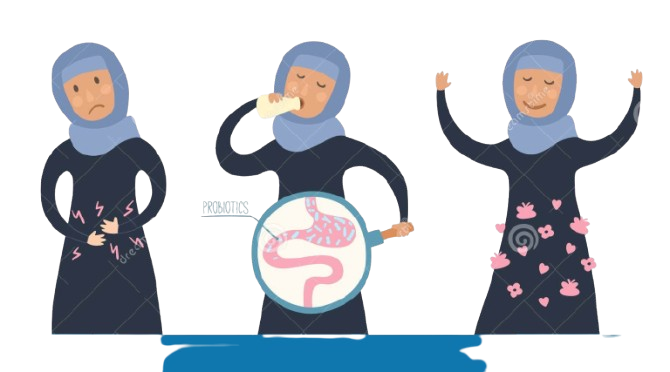
Supportive methods that complement mainstream medicine and help the overall recovery:



Clostridium difficile infection may feel like a storm in your gut—but with the right support, it doesn’t have to become a long-term crisis. Conventional treatments like vancomycin or fidaxomicin are important first steps. But for recurrent or resistant cases, Gut Microbiota Transplantation (GMT/FMT) offers a game-changing option that addresses the root cause: gut dysbiosis.
At Resplice, our holistic model combines state-of-the-art GMT, rigorous screening, and integration with immune support and lifestyle care. Our goal is to restore not just your gut health but your full body resilience—supporting the gut-brain axis, boosting immunity, and helping you recover mentally and physically.
Every infection has a beginning and an end. With the right treatments—and sometimes a little help from friendly gut microbes—you can get back to living, learning, and thriving.
Yes—through contaminated surfaces or hands. Hospitals must be especially vigilant with hygiene and cleaning.
Symptoms often appear during treatment or 1–3 weeks afterward, though later onset is possible.
Not necessarily. Mild cases can be treated at home under medical supervision with oral antibiotics and hydration.
Yes—up to 25% of people relapse. That’s when GMT or extended therapy is helpful.
Not enough to clear an infection alone—but useful as a preventive measure after antibiotics or combined with other strategies.
Severe or untreated cases can cause toxic megacolon or perforated colon—yes, potentially life-threatening.
Some, like clindamycin and broad-spectrum cephalosporins, carry higher risk. Always ask your doctor about alternatives.
Yes—especially if bathroom hygiene is poor. Always wash hands thoroughly and disinfect surfaces.
When done with proper screening and medical supervision as in GMT, it’s considered safe and highly effective.
Many feel improvement within days. Long-term gut stability may take several weeks as the microbiome settles.
Yes, though less common; antibiotic exposure or hospital stays increase risk—even in teenagers.
Not directly—but ongoing gut issues and poor diet can worsen gut dysbiosis, raising vulnerability.
Use antibiotics only when necessary, wash hands well, and support gut health with fiber-rich foods.
Yes, chronic diarrhea and gut inflammation can contribute to mood changes or fatigue.
Light activity and hydration support recovery—you don’t have to stay bedridden unless severe dehydration or illness.

Resplice Institute is India’s first integrated center offering autism therapy, gut microbiome treatment, and preventive health planning. We combine science and empathy to heal lives from the root.
© 2025 respliceinstitute.com || All Rights Reserved